Balance
THE EAR INSTITUTE OF TEXAS PROVIDES Balance Testing
HOW BALANCE WORKS
Balance and Coordination
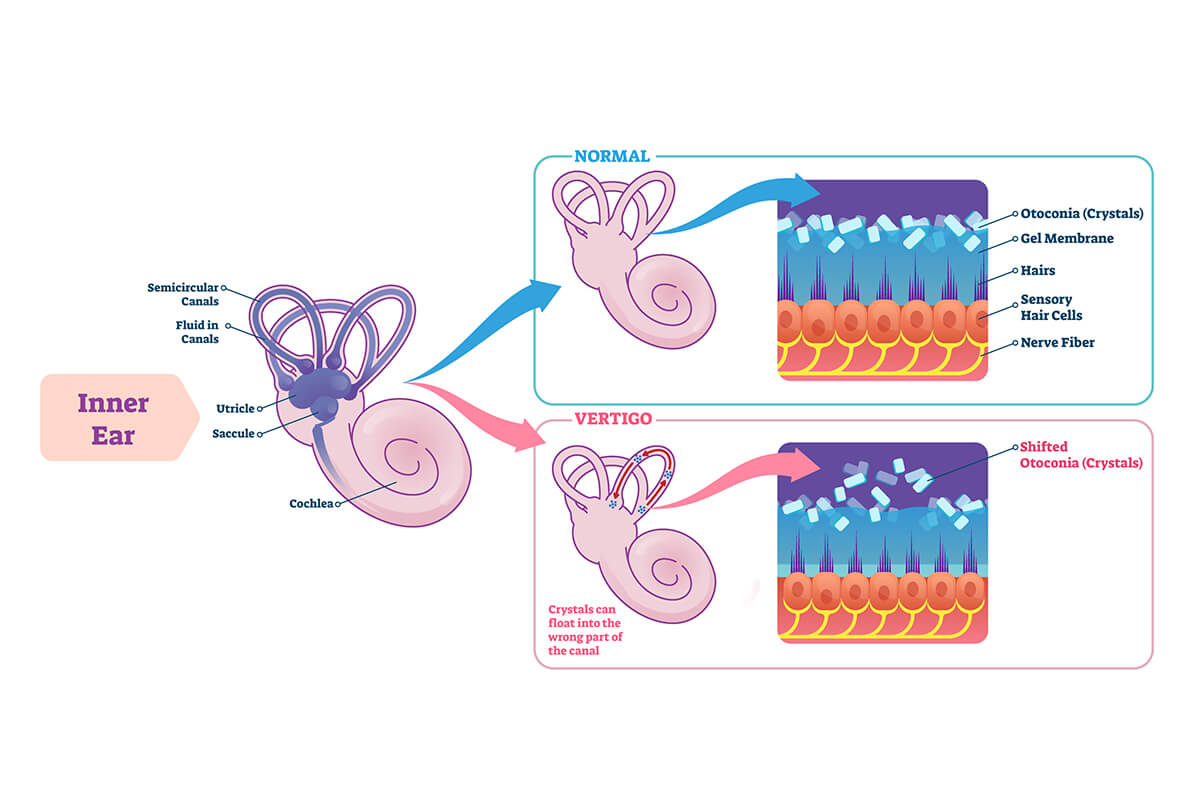
The vestibular system (inner ear) is also called the labyrinth. It monitors our directions of motions during turning, moving forward-backward, side-to-side, and up-and-down. The inner ear contains two individual organs for balance: (1) the utricle, made up of macula and saccule, and (2) a set of three semicircular canals.
The organs of the utricle are responsible for the sensation of gravity. The macula and saccule are made of delicate nerve endings that are connected to a structure made of calcium carbonate. These particles have a greater density relative to the fluid that they are immersed in, causing them to “fall” because of the action of gravity. As the head moves in relation to gravity, the particles exert pressure on the nerve endings (the best example of this is feeling the acceleration and deceleration in an elevator). The macula and saccule are roughly at right angles to each other and give slightly different positional information. In this way, the utricle of the inner ear is able to provide the brain with information about the position of the head relative to gravity.
Information on head rotation is provided by the semicircular canals. There are three semicircular canals in each ear: superior, horizontal, and posterior. They are roughly at right angles to one another; each one corresponding to one dimension in a three dimensional space. The canals are filled with a fluid. As the head turns, the fluid rotates within the canal and moves hair cells connected to nerve endings within one end of the canal. Fluid within the canals always moves in the opposite direction in each ear. The best way to explain this is: our ears are on either side of our head and if we turn our head, one ear goes forward and the other backward. This holds true with the fluid in the ear, it always moves in the opposite direction and the brain understands these signals as a coordinated movement. The nerve endings within the canals then send information back to the brain about how quickly and in what direction the head is moving. Try this, close your eyes and move your head a very tiny, tiny bit; almost keeping your head still and you should be able to sense even the very smallest of movement with your three semicircular canals in any direction. This is a very delicate system.
The visual system (eyes) monitors where the body is in space (i.e. upside down, right-side up, etc.) and also the directions of motion. Vision provides necessary information to the brain about our relationship to the environment. As we move and see how objects in our world are changing, our brain calculates our body’s relationship to those objects. The best example of this is looking over a cliff; we feel as though we are falling, even though our bodies are stable.
It is our eyes that are pulling us into our visual field; this is where our vestibular and proprioception systems try to overcompensate the signals to the brain, telling us that we are not really falling into the open space. Additionally, there is an intricate communication between the vestibular system and the movements of the eyes, the vestibular-ocular reflex (VOR). The vestibular system works to control eye position and movement so that when your head moves, your eyes can automatically stay fixed. VOR is easily explained; when you walk, your head moves up and down, but your visual world stays stable (unless your VOR fails, in which case you have oscillopsia or bouncy vision). Because of the vestibular-visual link, vestibular system problems can also cause fuzzy vision, nystagmus (abnormal eye jerking), and other visual sensations.
As seen above, the three primary balance systems: vestibular, visual, and proprioception individually send signals to each other as well as the brain about head and body movements relative to gravity and rotational movements.

To help overcome balance problems due to impaired vestibular function, the brain needs to receive additional information from the visual and proprioceptive systems while the vestibular system is being stabilized. The more signals the brain receives from the two remaining systems, the better your balance will be. Some suggestions for improving signal strength and interaction from vision and proprioception systems include:
- Use your eyes as much as possible.
- Place nightlights in bedrooms, halls, and bathrooms.
- Train your leg muscles and increase signals from both the legs and feet by walking barefoot on a variety of uneven surfaces (grass, sand, trails, hills, etc.).
- Practice sitting on a narrow beam with your feet dangling in the air. This helps your hips and upper body to help the legs to maintain balance. Again, use a partner.
- Swim with the eyes open, wearing goggles if necessary.
- Increase your muscle strength with exercise and sports (wear good, stable, flat laced shoes).
When it is dark, use a flashlight. The reasons are obvious: we cannot see very well in the dark, so the brain only receives signals from the muscles; this makes the person unstable. It is apparent that the brain has an incredible capacity to improve balance by finding new pathways and developing new strategies when one or two of the systems are impaired. This helps to explain why some patients benefit from balance therapy and rehabilitation.
BALANCE DISORDERS
About Imbalance
The dominant driving force to maintain balance originates from the inner ear. However, imbalance can result from a wide variety of causes, the most common of which occur as a result of the vestibular system (inner ear), visual system (eyes), or somatosensory system (body awareness) disorders. The somatosensory system involves touch, pressure, and joint position sense. Each system is an individual sense and has a responsibility to send information to the central nervous system (CNS), which is primarily the brain and cerebellum. Vestibular input sends information regarding our movements in relation to our postural control; our visual system sends information regarding our visual world; and the somatosensory system sends information pertaining to our contact to our exterior environment (our feet on the ground is the best example). If all of these systems are coordinated, we are stable and balanced.
There are some cases where the peripheral systems are working correctly: however, the patient may be having symptoms of dizziness and vertigo due to problems in the central nervous system. In these cases, our physician must evaluate many factors: are the signals not reaching the CNS, are there disease processes within the CNS, or are the output and reaction signals not function properly? Below are a number of potential possibilities that our physician can address, either through treatment or referral.
Cervical Vertigo
Cervical vertigo may be due to inflammatory and/or degenerative changes in the cervical spine or neck musculature. The neck muscles are constantly sending nerve impulses to the balance centers of the brain to help maintain equilibrium. Spasm (tenseness) of the muscles can result in an abnormal nerve discharge, leading to unsteadiness or dizziness. In this case a referral to a spine specialist may be necessary to resolve the underlying condition.
Circulation Changes or Vertebrobasilar Insufficiency
Circulation Changes or Vertebrobasilar Insufficiency (VBI) may cause dizziness; this is predominately due to decreased blood flow in the vertebral vessels when the head is turned in a particular position. Any interference with the circulation to the delicate inner ear structures or their central connections may result in dizziness, at times with hearing loss and tinnitus. Blood vessel spasms may cause sudden onset dizziness. Spasms result from certain drugs such as caffeine (coffee) and nicotine (cigarettes). Migraines may cause nausea, vomiting, and other neurological symptoms. Small vessel disease involved with aging in the brain stem also causes complaints of disequilibrium and/or gait instability.
Tumors
Acoustic Tumors or Skull Base Tumors cause hearing loss, tinnitus, and dizziness along with other neurological symptoms in the later development. These are usually benign tumors involving the hearing and balance nerve which usually affects only one ear.
Our Approach
Here at Ear Institute of Texas (EIT), we objectively evaluate each patient as an individual to determine the extent and specific nature of their concussion. The physician at EIT has specialized fellowship training in both neurotology and otology, and utilizes the latest medical advances to objectively evaluate each patient individually, addressing their concussion through a multi-dimensional approach to both diagnostic testing and treatment. EIT has adopted the most widely used and accepted methods of evaluation and treatment, combining them with technological advances to establish a concussion protocol that allows for an approach that focuses on the causes of the symptoms rather than the symptoms themselves. As a result, patients can have a faster and safer return to activities of daily living.
Concussions
A concussion is defined as an immediate acceleration, deceleration, or stopping event causing temporary or permanent damage to the structures of the head. The symptoms of a concussion can indicate both the mechanism of the injury and the specific structures within the head that may be damaged. Symptoms can include: disorientation, dizziness, nausea, “blurred” vision, loss of coordination and concentration, amnesia, and loss of consciousness.
When people think of a concussion, their first instinct is to think of brain trauma, which is not always the case. There are other structures within the head that are considerably more sensitive and more easily damaged than the brain, for example the vestibular system.
The brain has a considerable amount of protection from the structures around it, and is generally associated with immediate and severe symptoms. It does takes a great amount of force to damage the brain, and these injuries are usually seen in motor vehicle accidents or other high speed or high velocity events. They do occur in sports, but their frequency seems to be lower than initially thought. The vestibular system (inner ear) on the other hand is rather easy to disrupt in comparison to the brain, and current research is providing some evidence that a large portion of concussional injuries are actually damage to the inner ear or vestibular system, rather than the brain. A majority of common symptoms: headache, dizziness, nausea, blurred vision, and coordination and concentration problems that are associated with a concussion can be directly and in some cases solely attributed to the vestibular system. Only in recent years, with advancements in medical technology, have we been able to accurately and objectively evaluate the vestibular system, which is why it is considered one of the most misunderstood organs of the body.
Due to the potential involvement of various systems, it is quickly becoming the standard of care to treat a concussion from more than one perspective. Concussions should be evaluated with the understanding that there are different types of concussions. No two concussions are the same and they need to be evaluated on individual basis.
The different types of concussions
- Vestibular concussions (inner ear)
- Cerebral concussions (brain)
- 1. & 2. A combination of both (inner ear and brain)
Both vestibular and cerebral concussions have similar symptoms, making it difficult to distinguish. Therefore, the key to treating a patient is distinguishing between the different types of concussions and accurately diagnosing each injury. Advances in medical technology and diagnostics allow specially trained physicians the ability to view a concussion through its many causes and subsequent symptoms. Keeping in mind that the treatment for each is significantly different, and treating one concussion like the other may slow or prevent a full and safe recovery.
Sports Related Injuries
Sports related concussions generally occur in collision/contact sports such as football, ice/field hockey, basketball, and soccer. However, their impact is also seen in sports ranging from baseball to gymnastics and all recreational sports. When the head is put through a forceful and immediate stopping or starting, structures within the head can be damaged.
Diagnosis
The diagnosis of a concussion is made by a combination of historical information, physical examination findings, and diagnostic testing that includes: postural sway analysis, vestibular ocular reflex testing, audio-vestibular testing, and occasionally imaging techniques to include a CT or MRI scan. Both the central nervous system and balance system are evaluated using a combination of testing techniques. This testing protocol will identify any damage or weaknesses in the vestibular system, visual system, proprioceptive (sensation) system, and/or coordination and reflexes of the brain. There is a characteristic pattern for the evaluation of concussion: central nervous system concussions will present both objectively and subjectively different than a vestibular concussion. Vestibular concussions will have a very predictable abnormality, showing a specific correlation within a number of the diagnostic tests, allowing for an accurate identification of each injury.
Treatment
The treatment for a concussion will vary greatly for each individual, as each injury is significantly different and can fluctuate in both the severity and duration of symptoms. As a result, our physician and team of professionals will individually evaluate each injury, focusing treatment protocols on the causes of the symptoms rather than the symptoms themselves. Medical treatment will include the stabilization of the injury, in some cases with medication, rest, or specialized vestibular therapy.
The aim of treatment is to prevent the symptoms of a concussion from worsening (as they initially do over the first three day period), and then preventing them from having a negative impact on life. If a concussion is seen within the acute period (generally the first 12-72 hours), a majority of the lingering symptoms can be prevented from occurring. After this acute period, if no treatment is given, the central nervous system (CNS) and other systems begin to compensate for the injury, creating periods of “good days” and “bad days”. This cycle can continue for days, months, or years. A concussion having long lasting effects is commonly referred to as the post-concussion syndrome and can be treated with a similar methodology: stabilization of the vestibular system and retraining of all the sensory input systems. The process of retraining a stable vestibular system is to allow the sensory systems of the body to more effectively coordinate their individual activities with one another and the external environment. As a result, treatment protocols are very individualized and are tailored for each patient based on their specific needs; no two treatments will be the same, nor will two patients respond in the same way.
Definition
The labyrinth is the medical terminology for the balance portion of the inner ear. The inner ear consists of a complex area in the temporal bone and can be divided into three parts: the vestibule (in the middle), cochlea (in front), and semicircular canals (in the back). All three parts form a continuous and tortuous space containing different fluids (endolymph, perilymph, and cortilymph), and each are separated by delicate membranes. The hearing portion of the inner ear is the cochlea. The balance portion, or labyrinth, consists of the vestibular endorgans in the semicircular canals . Any abnormality that is related to either the function of the labyrinthine or the labyrinthine sensors is considered a labyrinth dysfunction. In most situations with labyrinthine dysfunction, the labyrinth does not properly respond to movement changes of the body.
Causes
The causes of labyrinthine dysfunction can vary greatly: however, some of the leading causes are:
- Prior ear surgery (Less frequent with newer techniques)
- Head trauma, including whiplash injuries
- Barotrauma (scuba diving or sudden pressure changes to the inner ear)
- Acoustic trauma
- Idiopathic or unknown cause without any underlying factors
Diagnosis
The diagnosis of labyrinthine dysfunction is based upon both the patient’s subjective complaints and diagnostic testing. Generally, patients will complain of vestibular symptoms, (vertigo-with or without head position changes, dysequilibrium, motion intolerance, nausea, and vomiting), disorganization of memory and concentration, and/or perceptual disorganization in complex surroundings such as crowds or traffic. Diagnostically, patients will present with abnormal positive test results for vestibular dysfunction. The patient may not be able to stand with their feet together (Romberg test) and remain still, nor are the able to perform a more difficult test of having the feet heel-to-toe (Tandem Romberg).
Diagnostic Testing
There are a number of tests that can be helpful in identifying the exact nature of a patient’s labyrinthine dysfunction.
Neurotologists at EIT may use: ENG, ECoG, Audiogram, or ABR testing. Additional testing may include a CT scan or MRI scan.
Treatment
The final diagnosis is made by your physician who will evaluate both the symptoms as well as the causes of the symptoms. Treatments can range from medical therapy, home exercises, physical therapy, or a combination. In a few cases, surgery may be needed to resolve the dizziness.
About Motion Sickness
Motion sickness, or seasickness, is usually just a minor annoyance and does not signify any serious medical illness. Some travelers are incapacitated by it, and a few even suffer symptoms for a few days after the trip. About one third of the population is highly susceptible to motion sickness. Some experience symptoms in fairly rough conditions, and others become sick only in extreme conditions. Some groups that seem to be particularly more susceptible to motion sickness include: children aged 3 to 12 years, people who suffer from migraine headaches, and women during menstruation and pregnancy.
Early signs of motion sickness include pallor, restlessness, and cold sweat. In later stages, nausea, excessive salivating, and vomiting can occur. The degrees of symptoms that result from an acute exposure to provocative stimuli vary with the intensity of the stimulus and each person’s susceptibility to this condition.
Motion sickness occurs when the sensory inputs (vestibular, visual, and/or proprioception or “body sense”) sends information about the body’s position that contradicts what it is perceived to be experiencing. Sometimes the incoming signals from these sensory sites conflict with each other; other times these signals conflict with the brain’s “positional memory.” It can be brought on by abrupt changes in movement, such as during bumpy rides, turbulent flights, or rough seas. It can also occur when one is exposed to moving visual scenes while the body is in a relatively fixed state. Another new theory for some cases of motion sickness is the postural instability theory. This theory is based on experiments in which motion sickness was preceded by statistically significant increases in postural sway, indicating an underlying vestibular abnormality and a decreased ability to actively control the body’s postural motion.
Treatments for Motion Sickness
Prevention in most cases is accomplished by seeking areas of lesser movement in an interior location of a large ship or by facing forward and looking outside a ship or plane at a stable horizontal line. Several medications are available, by prescription or over the counter, such as Valium, Antivert, and Dramamine that prevent or limit the symptoms of motion sickness. If medications are necessary, they are best taken at least one hour before embarking. For longer trips, a prescription medication, called Transderm-Scop, can be worn behind the ear, for up to three days at a time.
Additional Information
In some cases, motion sickness may have other underlying causes associated with vestibular dysfunction. These causes may be linked to Meniere’s disease, chronic imbalance, chronic ear infections, benign paroxysmal positional vertigo and others. Please always consult your physician about your symptoms; early intervention is the best way to prevent progression, if an underlying problem does exist.
What is Meniere’s disease?
Prosper Meniere was a French Physician who described a new disease process in the mid-1800’s. The disease he identified consisted of four symptoms: attacks of vertigo, ear fullness or pressure, low-pitch tinnitus (ringing), and fluctuations in hearing. At the time, the cause of the ailment was unknown, but Meniere believed that it originated within the ear. Since that time much has been learned about the disease and its treatment; interestingly, however, we still do not know the cause of the disease Meniere described. There are now known to be multiple variants of this disease process, with similar pathologic consequences (abnormal tissue changes). Some forms affect only hearing, others only balance, and still others have a few, but not all, of the classic four symptoms. The classic four symptoms of Meniere’s disease are: severe vertigo with imbalance, fluctuating hearing loss, tinnitus, and ear pressure sensation.
Histopathology
It has been well characterized since the 1930’s, that all forms of Meniere’s disease involve enlargement of the scala media portion of the inner ear due to elevated fluid pressure, causing bulging of the surrounding reissner’s membrane. Eventually, the membrane ruptures with mixing of endolymph and perilymph (inner ear fluids), causing injury to the hair cells and producing the characteristic symptoms. This process is called “endolymphatic hydrops”, meaning too much endolymph. Only the classic symptom complex described by Meniere himself should be referred to as Meniere’s disease, whereas all the other forms are more properly termed “hydrops”, or “endolymphatic hydrops”. The precise cause of the excessive fluid is unknown and whether it is due to an overproduction of endolymph or an under-resorption is debated. Either way, the net result is too much endolymph with distressing symptoms. Although the etiology (cause) of “Meniere’s disease” is unknown, there are many known triggers of endolymphatic hydrops. These include allergy, immune mediated, metabolic disorders, infections (syphilis), congenital malformations of the ear, and trauma. The known causes occur infrequently compared to the idiopathic form (unknown cause), but a search is often undertaken.
Diagnosis
The discussion you have with your Ear Institute of Texas physician is the most important aspect of making the diagnosis. The vertigo spells are classically episodic, not occurring more than once a day, and often separated by days, weeks, or even years. Vertigo (sensation of motion) in hydropic attacks can occasionally be heralded by ear fullness, an increase in ringing (tinnitus), or a sudden drop in hearing. Rarely, an improvement in hearing precedes the attack (Lermoyez syndrome). The attack typically lasts anywhere from 20 minutes to an entire day, depending on how long it takes for Reissner’s membrane to repair itself. The vertigo is typically described as a spinning sensation (either the environment or the individual is perceived as spinning), which is quite disabling, and often associated with severe nausea and vomiting, sweating, and occasionally loss of bowel and/or blander control. They are not associated with severe headaches. The Tumarkin variant of hydrops has sudden loss of postural control with “drop attacks”, and is thought to be due to involvement of the otolithic component of the inner ear. After an attack of vertigo, one may experience a period of unsteadiness lasting for hours to weeks (occasionally years) as the brain compensates for the loss of balance function.
Hearing loss in hydrops is quite variable, ranging from a sudden, severe loss without return of function, to a gradual decline over months to years. The most typical pattern is that of hearing fluctuations, with periods of good and poor hearing, associated with a gradual decline in word recognition. The classic form of Meniere’s disease consists of a low frequency loss during an attack that may (or may not) return to normal afterwards. Essentially, any pattern of hearing loss may be associated with hydrops; therefore, the audiometric pattern can not be solely relied upon to make the diagnosis. A demonstrable fluctuation in hearing in one ear or the other helps to make the diagnosis of hydrops.
Classically, low-pitched roaring sound is heard in the affected ear prior to, or during, an attack of vertigo. This too is highly variable, and some individuals may experience constant ringing (tinnitus) in the ear. The precise etiology of the tinnitus is poorly understood, but thought to arise from a loss of usually spontaneous activity of the cochlear hair cells. A sensation of fullness or pressure in the ear may accompany the vertigo attack as well. This is thought to arise from over-distension of the endolymphatic compartment with injury to the hair cells.
Not unusually, patients with hydrops are quite sensitive to changes in barometric pressure and may experience more attacks in the spring and fall. Hormonal changes that occur during menses and pregnancy may trigger an attack. Tension, stress, anxiety, allergy, and exhaustion are also known triggers of an attack.
Testing
A long list of disease processes must be excluded prior to making the diagnosis of hydrops or Meniere’s disease. Tests of hearing, balance, and occasionally imaging are often performed. Pure tone and speech audiometry, as well as electrocochleography (ECoG), are routinely performed at the Ear Institute of Texas. The former is a standardized hearing test, while the latter is a more specific test of inner ear fluid balance. Balance and vestibular function testing are also completed. When the diagnosis of hydrops is entertained, an ABR, or MRI/CT scan (imaging studies) is sometimes performed to ensure that the symptoms are not being caused by a tumor. It has been shown that nearly 1 patient in 10 with a tumor on the balance nerve will demonstrate “classic Meniere’s symptoms.” This does not mean that 1 out of 10 people with hydrops has a tumor, as these tumors are exceptionally rare, yet it remains an integral part of the diagnostic workup.
Medical Treatment
Once a diagnosis of Meniere’s disease is established, non-surgical treatments are attempted as first-line therapy to control the vertigo and other symptoms. Lifestyle modifications are recommended, including a low salt diet, reduction/avoidance of caffeine and alcohol, and control of stress. Medications such as a diuretic (water pill) may be prescribed to eliminate excess fluid. Since Meniere’s disease can be precipitated by environmental and food allergies, allergy testing and treatment are often recommended and performed at the Ear Institute of Texas. While medications can be given during times of disabling vertigo episodes (e.g. Meclizine/Antivert, Phenergan, and Valium), it is best to otherwise avoid vertigo suppressant medications since they can delay overall recovery. Vestibular rehabilitation by a specially trained therapist has been proven to be extremely useful in speeding recovery and improving balance, and is frequently prescribed by the Ear Institute of Texas physicians.
Surgical Treatment
Meniere’s disease is a prominent cause of recurrent dizziness attributed to the inner ear. For those patients who suffer from the disease, the symptoms can be life altering and dramatically affect ones ability to function in normal daily living. The treatment of Meniere’s disease has evolved over many years. New minimally invasive techniques utilizing the use of endoscopes and/or lasers have become available that are generally well tolerated and even allow the patient to self-treat the inner ear under the direction of the neurotologic physician.
For more information about the surgical treatment of dizziness and Meniere’s disease, please click the following link: Surgical Treatment of Dizziness and Meniere’s Disease.
Physical Therapy
Often, the balance system has been permanently damaged by the vertigo attacks from Meniere’s. This creates a chronic sensation of imbalance or lightheadedness. Vestibular rehabilitation therapy has been proven to be highly effective in relieving these symptoms by improving the central balance system (within the brain). A specific program is designed to improve the weaknesses of your balance system, which may include problems with vision, proprioception, and vestibular input. Vestibular rehabilitation therapy is often combined with other therapeutic modalities such as medications, allergy immunotherapy, or surgery.
Prognosis
Hydrops is a chronic disease, like diabetes or hypertension. It needs to be treated medically (low sodium diet and diuretic) like other disease processes for many years. Like other disease states, it is can often be well controlled with medical therapies. This fact needs to be taken into account when surgical options are entertained. Certain individuals with hydrops will develop the disease in the opposite ear, which occurs in 5-30% of patients with hydrops. If an individual has had Meniere’s disease in one ear for three or more years, without symptoms in the other ear, the likelihood of getting dizziness in the other ear is quite rare. The vertigo associated with hydrops can burn out over time (usually a several year period). Your Ear Institute of Texas physician will do everything possible to allow you to live free of Meniere’s symptoms.
Meniere’s Disease/Endolymphatic Hydrops
Understanding the basic anatomy, function of the human ear, and the mechanism of balance and hearing are important pieces of information when addressing the many underlying causes and symptoms ear disorders. Many other disease processes are related to the ear such as: Migraine Disease or Labyrinthine Dysfunction.
Migraine Disease
About Migraine Disease
Migraine disease is a complex neurologic disorder in which headache is but one symptom. The disorder is usually inherited, and is extremely common. About 18% of women and 6% of men have the disease, although less than half of them are aware that their symptoms are migraine related. The disease has been categorized as Migraine with Aura and Migraine without Aura. The aura is a transient, usually reversible neurologic dysfunction. Although headaches are very common in migraine patients, they are not necessary to make the diagnosis. This type of migraine is termed a “migraine equivalent” or more properly, Migraine Aura without Headache. The disease tends to change throughout one’s lifetime, with headaches predominating at one time, and the aura at another.
The know association of dizziness and vertigo with migraine disease date back more then 100 years. 33% of migraine patients will experience true vertigo at some point in their lives, 72% will have dizziness, lightheadedness, or unsteadiness. Migraine disease is one of the more common causes of dizziness in children. Visual motion intolerance and motion sickness are frequent in migraine sufferers. Vertigo may be positional, spontaneous, or induced by stress, hormonal fluctuation, allergies, as well as certain foods or chemicals.
In addition to vertigo and dizziness, migraine disease can cause a variety of symptoms. Hearing loss, tinnitus, aural pain, visual loss, nausea, vomiting, imbalance, and blank outs are all possible. The vast majority of patients experience these symptoms independent of their headache.
Pathophysiology
Migraine is thought to be the hereditary manifestation of abnormal sensitivity to neurovascular changes. Simply stated, there is an abnormality in the part of the brain controlling or modulation incoming signals. Two theories are accepted: 1) neurovascular theory of inflammation and 2) serotonin deregulation. The first mechanism implies the presence of an irritable pain generator in the brain stem. When this is triggered, the trigeminal nerve releases inflammatory chemical substances (i.e. peptides) into the brain. The peptides cause a leakage of the meningeal blood vessels in the brain, causing them to distend, which result in inflammation and pain. According to the second theory, when an adequate trigger is received, serotonin platelet levels drop, and a headache ensues. Changes in hormonal level, sleep state, diet, altitude, stress, and allergy may each alter the amount of chemical neurotransmitter released from one nerve terminal to the next. The stimulus is thus amplified beyond that of the primary event. When these changes are occurring on a blood vessel, spasm ensues. Such vasospasms are thought to be responsible for the sudden hearing loss and blindness that can happen with migraine. When they occur on a nerve terminal, the normal function of the nerve is altered dramatically, causing symptoms like vertigo, motion sickness, and pain.
Diagnosis
The diagnosis of migraine disease causing dizziness is made by a combination of historical information, physical exam findings, laboratory data, audio-vestibular testing, and occasionally imaging (CT or MRI). A family history of migraine disease is often a strong predictor of migraine as the diagnosis. The entire balance system is evaluated using a combination of tests, which identify any weaknesses in the inner ear, visual system, proprioceptive (sensation) system, and the brain. There is no characteristic pattern for migraine disease, but the absence of other processes makes the diagnosis more likely. Concern for an intracranial process (stroke, tumor, MS) may prompt an X-ray evaluation with either a CT or MRI scan.
Treatment
Management of this disease process has many levels. Known triggers of migraine should be eliminated, such as nitrate/nitrite containing foods, sulfites, caffeine, aspartame, nuts, and certain fruits. Stress management can be useful for some, and regular sleep and exercise are also very important. Allergic trigger are extremely common, and formal allergy testing is often performed, followed by immunotherapy. Both inhalant allergy and food allergy are important to eliminate. Pharmacological management is often essential to obtain initial control of the disease. Many different classes of medications can be utilized, all with the same common goal to reduce neurotransmitter levels. Medications include: Verapamil, Midrin, Paxil, Elavil, Triptans and others. Triptans act on the 5HT-ID receptors on the nerve terminal to decrease the release of peptides, and on 1B receptors of the meningeal blood vessel to reduce vasodilation and leakage. Some of these medications are also used to treat depression, and often that can be useful given how debilitating this disease can be. The primary focus of their use is, however, management of neurovascular abnormalities causing the symptoms of migraine. The duration of medication therapy can range from 6 months to several years. Lastly, migraine may cause constant disequilibrium and balance problems, which are addressed with a specialized form of physical therapy, called vestibular rehabilitation. This is highly effective in eliminating these symptoms.
Foods to Avoid
- Avoid Caffeine: soda, coffee, tea, chocolate
- Eliminate nitrate/nitrite: wines, hams, bacon, sausage, lunch meats, hot dogs, red wine.
- Avoid large quantities of cheese, especially aged and cheddar (American, cottage, cream and velveeta are okay)
- Avoid Monosodium Glutamate (MSG), found in Chinese food (read labels and ask server to leave out of prepared dishes)
- Avoid Aspartame is found in artificial sweeteners (Nutrasweet and Equal)
- Avoid consumption of large quantities of nuts
- Limit citrus fruits to 1 serving per day
- Avoid skipping meals, prolonged fasting, or excessive ingestion of carbohydrates at a single sitting. Establish a routine sleep-wake cycle. Get regular exercise, avoid extreme exertion or fatigue.
Superior Semi-circular Canal Dehiscence
About Superior Semi-circular Canal Dehiscence
On occasion there is an absence of bone over the superior semicircular canal. When this entity is present, it causes a syndrome in which balance abnormalities occur as a result of hearing loud noises or experiencing pressure changes in the ear.
This syndrome produces some very specific symptoms. Patients can experience vertigo (an illusion of motion) caused by noises or pressure in the ear. The noises that can provoke such symptoms include loud music, being in a noisy environment such as a sports event, sounds on the telephone such as the dial tone or a busy signal, and sounds made by the patient such as singing at certain pitches. The pressure symptoms that can provoke the symptoms include pushing on the outer aspect of the ear, blowing through the nose while pinching the nostrils, and straining while lifting heavy objects. In addition to these symptoms that occur in specific association with the stimuli just described, patients with this syndrome may experience a generalized and more constant sense of disequilibrium and unsteadiness.
Surgical Procedures for Superior Semicircular Canal Occlusion
A Middle Fossa Craniotomy is performed affording access to the base of the skull and the superior semicircular canal. The canal is plugged thus alleviating the source of balance disturbance associated with this syndrome.
